In its long and venerable history dating back 192 years, the British Medical Association used to shy away from being called a “trades union”.
Collective bargaining was for “trades people”; the doctors were independent professionals. Their association was there to campaign for best practice and to offer advice to the politicians regulating health treatment.
That was when the reflex of most medical practitioners was to subscribe to the Hippocratic principle often paraphrased as “first do no harm”.
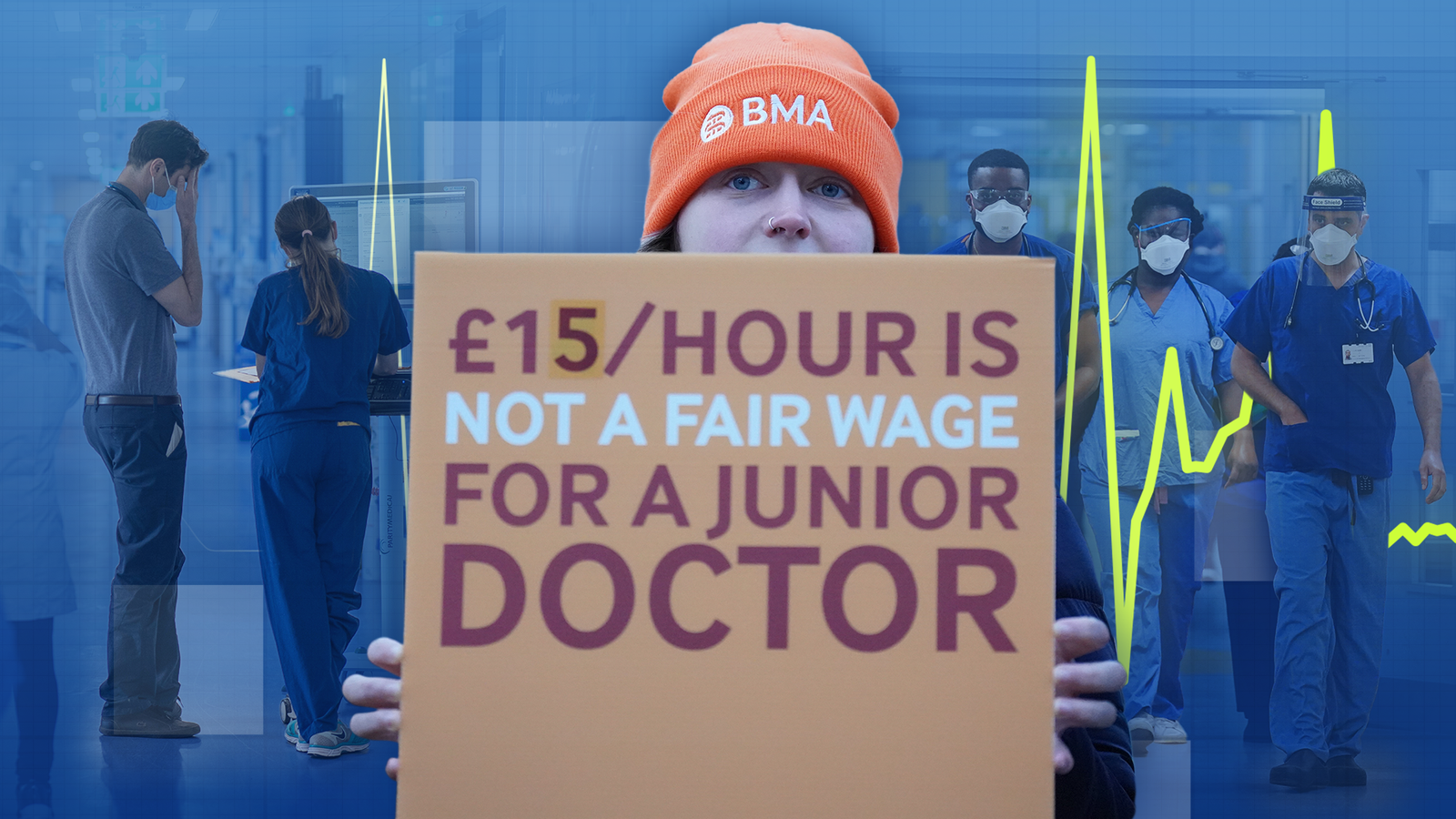
Much has changed. Today the BMA has no qualms about being described as the “doctors’ union”.
It has freely employed strong-arm negotiating tactics, familiar from industrial disputes, in pursuit of better pay for its members – including strikes, walkouts, deadlines and work to rules.
These have culminated in the current “unprecedented” six-day strike by junior doctors in England, which is due to end at 7am on Tuesday.
There can be no doubt that the strikes are doing harm to patient care.
NHS England has just reported that 89,000 “appointments and procedures” had to be put off because of the three-day strike in December.
Since the industrial action started last March, 1.2 million appointments have been cancelled and rescheduled.
The BMA rejected requests from the NHS to keep working in critical areas including fast-progressing cancers, corneal transplants and emergency caesareans.
Heated recriminations broke out as the BMA accused hospital managers of “weaponising” so-called “derogation requests” permitting them to recall staff to work if patient safety is “in jeopardy”.
Meanwhile, some A&E departments declared “critical” incidents with waiting times for treatment stretching as long as 16 hours.
PM failing to fix waiting list backlog
“Cutting NHS waiting lists” was one of the prime minister’s five pledges and this aim is seriously off track. Opinion polls taken during the dispute suggest that just over half of the public back the strikes (53%).
In a survey four months ago, people were more inclined to blame the government for the dispute (45%) than the BMA (21%), although 25% said they were both responsible.
Yet 11 months into the confrontation, the junior doctors, who lose pay on strike days, must be wondering what they are getting out of it. Their demand for a massive 35.3% pay rise still seems out of reach.
Having walked out of negotiations in December, Dr Vivek Trivedi, co-chair of the BMA junior doctors’ committee, now says he might be prepared to engage in more talks, saying “all we want is a credible offer that we can put to our members and we don’t need to strike again”.
Click to subscribe to the Sky News Daily wherever you get your podcasts
Although discontent over pay is widespread throughout the NHS workforce, most sectors other than junior doctors in England have accepted deals or, at the least, suspended their action.
NHS consultants accepted salary rises of up to 12.8% along with some pay reforms.
The Royal College of Nursing ballot for further strike action failed and a pay rise of 5.5% was imposed.
Health management is devolved. Junior doctors in Scotland accepted a 12.4% pay rise, on top of 4.5% in 2022/23. Junior doctors in Northern Ireland are balloting on a similar offer. In Wales, there is the prospect of a three-day strike from 15-18 January.
When negotiations broke down before Christmas, the government was offering a 3.3% increase on top of the 8.8% already imposed, taking the total for the English juniors above 12%.
Are the strikes really ‘saving the NHS’?
By the standards of the other disputes, a reasonable settlement should be within touching distance were it not for the sense of grievance, embodied in the claim that pay has been cut in real terms by more than a third since 2008.
Few independent analysts accept the BMA’s calculation, which relies heavily on RPI inflation fluctuations. In line with recent trends for national statistics, the independent Institute for Government says the CPIH, the consumer price index, would be a more appropriate indicator, meaning a cut of 11-16%.
This was in the post-credit crunch, austerity period when wages across the public and private sectors stagnated.
The public is sympathetic to junior doctors who help to keep them well, but should they be an exception?
Over time, pay structures change. The youngest and lowest paid of those now on strike were at primary school in 2008; is it rational to restore their pay levels to what they were then?
“Junior doctors” is an unsatisfactory catch-all term for a wide range of hospital doctors. “Doctors in training” – which some Conservative politicians attempted to popularise – hardly does them justice either.
The term covers all hospital doctors who are not consultants, ranging from those just qualified and still effectively indentured, to senior registrars.
Read more from Sky News:
‘Net may be closing’ on those responsible for Post Office IT scandal
Men jailed after using fake gun to try to steal Ferrari from ‘terrified’ couple
First-year junior doctors earn £32,398, rising to £37,303 in the second year and £43,923 in the third. Registrars’ basic pay goes up to £58,000. Full-time NHS consultants earn up to £120,000.
On the picket lines, strikers often argue their action is not about their own pay but to save the NHS because, they say, many of their peers are leaving for better terms in Australia, New Zealand and Canada.
Conversely, as recent special grade immigration figures show, there are many qualified people abroad with conflicting aspirations who are anxious to come here to work in the NHS.
Much to ponder on how the NHS should work
The additional crisis brought on by the strikes has inevitably prompted some rethinking about how the NHS is working.
Speaking to Sarah-Jane Mee on the Sky News Daily’s How To Fix The NHS mini-podcast series, Dr Adrian Boyle, president of the Royal College of Emergency Medicine, observed “that everything flowed better” in A&E departments because senior doctors providing cover had more direct contact with patients and “there were fewer people coming into hospital for elective work and this meant more beds”.
Those statements about organisation in the NHS should provide consultants, junior doctors and potential patients with a lot to ponder.
The same goes for politicians, who the public holds primarily responsible for delivering their healthcare.
Steve Barclay took an abrasively inactive approach to the various NHS disputes when he was health secretary. In November he was moved to make way for the more emollient Victoria Atkins.
She says she wants “a fair and reasonable settlement” to end the strikes and is open to further negotiations provided the threat of more strikes is withdrawn.
Is the NHS broken – and would Labour do any better?
Atkins’ position is not much different from Wes Streeting, her Labour opposite number.
He has said for months that the disputes should be sorted out by negotiations with ministers and that a Labour government would not meet the 35% pay claim.
Streeting is of the view that reform, likely to discomfort some of the NHS’s vested interests, is more needed than extra cash.
Whatever view they take of the doctors’ actions, public pessimism about the NHS is on the rise.
Much as they love the NHS, growing numbers of the public say it is “broken” or “not fit for purpose”. There is also a live debate about whether doctors should lose the right to strike, just like the police and members of the armed services.
The pollsters regularly ask the question “should doctors be allowed to strike?”
Last summer, at the height of the consultants’ dispute, 50% said yes, 42% no. By November, support for doctors’ right to strike had dropped to 47% yes, 46% no.
The asking of that question alone would have astonished the founders of the BMA’s precursor, the Provincial Medical and Surgical Association, back in 1832.