Exactly four years ago today the UK’s first coronavirus cases were confirmed.
On 31 January 2020, Public Health England said a University of York student from China had tested positive for COVID-19, along with his mother.
Almost two months later, the UK locked down and it was another two years until the final legal restrictions were removed – with some arguing this happened prematurely.
Now in 2024, the virus is still affecting people in ways scientists are only just beginning to fully understand – and affecting the NHS. So how prevalent is COVID today and what have we learned?
How widespread are COVID infections now?
Unsurprisingly, COVID cases are much lower than they have been at various peaks over the past four years.
But the latest data, which covers up to 10 January, estimates that 2.3% of the population of England and Scotland had COVID in the community – the equivalent of around 1.2 million people.
As people no longer report their test results, the most reliable recent estimates on COVID prevalence come from the winter infection survey, carried out by the Office for National Statistics (ONS) and the UK Health Security Agency.
It is smaller than the original, regular ONS infection study that was discontinued in March 2023, and it doesn’t cover Wales or Northern Ireland.
Although the winter infection study uses lateral flow not PCR tests, the results are broadly comparable.
It shows that following the spread of the JN.1 variant, which is a sub-lineage of the BA.2.86 version of Omicron, the virus last peaked before Christmas, with highs of 4.4% between 19 and 23 December – roughly one in 23 people.
Similarly to the height of the pandemic, the peak was felt most strongly in London, with 5.5% of the capital believed to have COVID by 19 December. The lowest peak was in the North East, with 3.2% of the region thought to have had the virus by 12 December.
Will we see more waves of cases?
The recent COVID peaks are only around half what they were in spring 2022, when 7.6% of England were estimated to have the virus and 9% of Scotland.
Stephen Griffin, professor of virology at the University of Leeds, warns that although the peaks look less dramatic, repeated waves mean they add up to a very high number of cases.
“We’re still seeing multiple waves of COVID every year because the virus is still evolving at an incredible rate,” he says.
The government often cites the initial vaccine rollout as the biggest success of its COVID response.
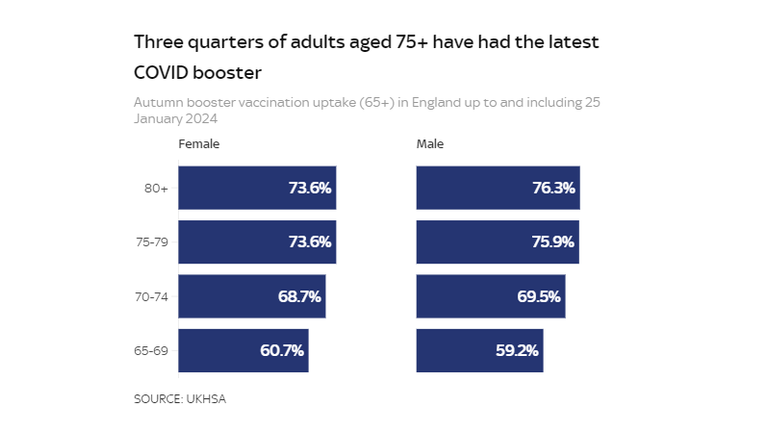
After they were offered to everybody aged 12 and over, 85% had two doses of a vaccine by mid-2022. But additional booster jabs are now only offered to the over-65s.
And with new variants constantly emerging and most people’s vaccine protection waning, Prof Griffin says the UK is “not suppressing prevalence”, which means “we’ll continue to see those waves”.
How many people have to go to hospital for COVID now?
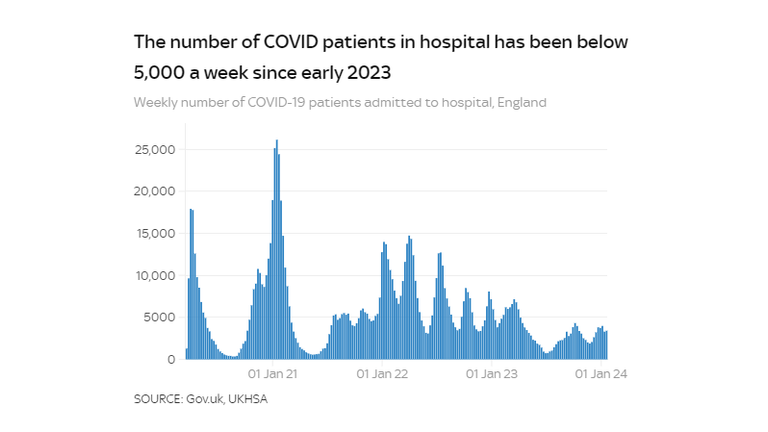
The pre-Christmas peak in cases didn’t result in as large numbers needing hospital treatment compared with the early days of the pandemic.
Professor Oliver Johnson, professor of information theory at the University of Bristol, says while there have been “many infections” recently, “they are much less severe on average since before we had vaccines”.
Fewer than 5,000 people with COVID have needed hospital treatment in England every week since early 2023. That number peaked at more than 25,000 in a single week in January 2021.
What impact has the anti-vax movement had?
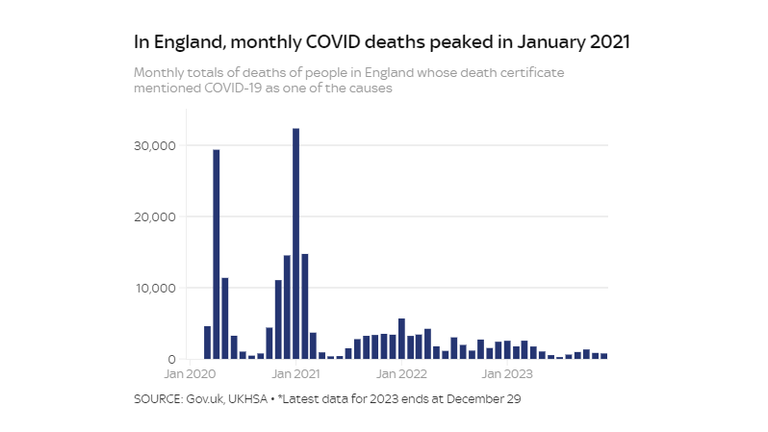
Far fewer people are dying with COVID than before vaccines were offered to all over-18s in June 2021.
Despite the pandemic sparking a resurgence in the “anti-vax” movement, Greg Fell, Sheffield’s director of public health, says the overwhelming positive impact of vaccines on COVID mortality has undoubtedly been “good PR” for them.
“Anti-vax sentiment clearly got highlighted during COVID – but I think most people know that those vaccines really work and that in a world without them, it would be Christmas 2021 again.”
Asked whether the recent drop in MMR vaccines and the measles outbreak in the West Midlands are solely the result of anti-vax groups, he admits there has been “some outright anti-vax sentiment” around MMR that has had an impact, particularly on social media.
But he stresses that addressing “missed opportunities” to use community leaders to engage with disenfranchised groups is just as important in reversing the problem.
Prof Griffin says the delayed decision to vaccinate five to 11-year-olds in 2022 was bad for jab rates, alongside the then-health secretary Sajid Javid’s description of the programme as “non-urgent”. Data shows only around 10% of under-12s had a single dose.
“The dithering and indecision around the benefits for vaccinating children was pretty damaging in the sense that if you look at uptake in younger groups, it’s appalling,” Prof Griffin adds.
Primary courses of the vaccine are also no longer universally available for all age groups, aside from the clinically vulnerable and people who live with them.
“So children turning five after September 2022 have to wait until they’re in their 60s to have a vaccine, unless they become clinically vulnerable,” Prof Griffin says.
“The idea that repeated infections are a preferable means of generating population immunity to vaccines, especially in children, is a dangerous nonsense.”
Concerns over ‘silent organ damage’ from COVID
Long COVID is defined by symptoms that persist for three months or more with no other explicable cause. Almost two million people in the UK had the condition at the time of the latest ONS survey in March 2023.
Studies have put the extra cost to UK GP and other primary care services at an estimated £23m a year – with annual losses to the workforce and greater economic cost thought to be as much as £1.5bn.
A Canadian study suggested that for people infected three times or more, long COVID rates were around 38%.
Dr Rae Duncan, a consultant cardiologist and long COVID research clinician at Newcastle Hospitals NHS Foundation Trust, warns that studies are beginning to suggest serious complications from COVID that could lie dormant for years.
“COVID is a spectrum and long COVID is only one end of that,” Dr Duncan says.
“It’s never been just a cold. The more times you’re infected, the higher your cardiovascular risk, neurological, and endocrine risk. These can all result in life-altering conditions.
“Some may have underlying silent organ damage, which is asymptomatic, meaning people are not aware of it. It needs more research but it’s very concerning.”
Read more:
How long COVID ruined my life
Hundreds of long COVID doctors suing NHS
A UK biobank study found increased risk of cardiovascular death up to a year-and-a-half after getting COVID in unvaccinated people. Others, including data pooled by scientists in Taiwan, show far greater COVID mortality in people with Alzheimer’s disease.
One piece of research suggested babies born to COVID-positive, unvaccinated mothers had a 20.3% risk of neurodevelopmental delay by age, compared to 5.9% of babies whose mothers did not catch COVID while pregnant.
Given emerging research the virus may carry cardiovascular risks for children, citing NHS guidance that children can go back to school three days after getting COVID, Dr Duncan adds: “We have published data showing it takes around seven days for 75% of children, and 10 days for 90% of children to become non-infectious.
“So we have largely chosen to ignore the impact of COVID on our kids and I think that’s a really bad decision.”
How many people are dying with COVID?
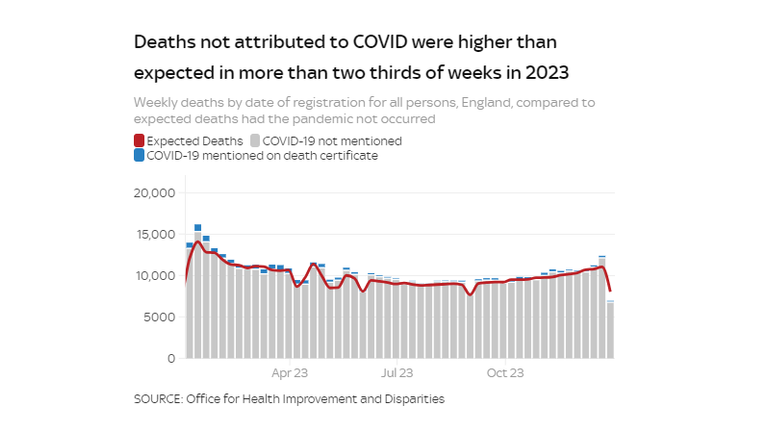
Last year excess deaths (how many more deaths occur than are expected) were still higher than the five-year average, but down on 2022 – from more than 30,000 in 2022 to nearly 27,000 in 2023.
COVID-related deaths almost halved from 32,300 in 2022 to 16,600 in 2023. But they still made up almost two-thirds (62%) of excess deaths last year.
Many argue that NHS backlogs are contributing to excess death numbers, and pressures are evident across all areas of services.
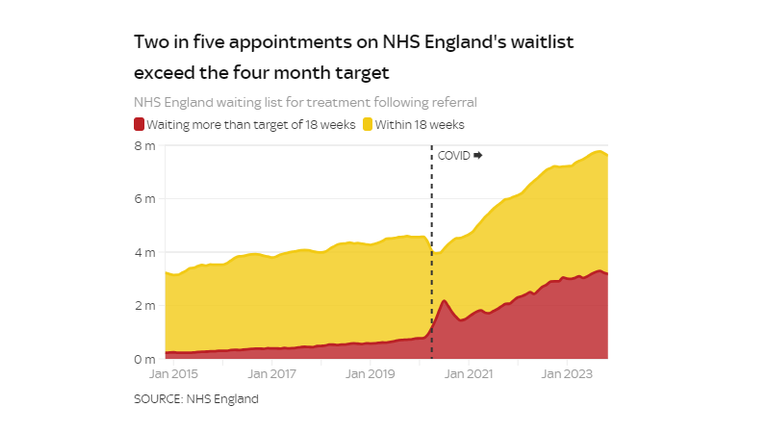
According to the latest data from November, 6.4 million patients were on the waiting list for treatment in England, 42% of whom were still waiting beyond the 18-week target.
The Royal College of Emergency Medicine attributed more than 23,000 excess deaths in England in 2022 to long waits in emergency departments – where the latest figures show nearly half (46%) are still waiting far longer than the four-hour target to be seen.
Prof Griffin says: “Excess mortality has got less attributable to COVID, but it’s still a problem.
“COVID did have a huge impact on NHS capacity to deal with the backlog, but we haven’t had those widespread restrictions for several years now, yet the NHS has been unable to catch up again and the year-long added pressure from COVID hospitalisations remains.”
Prof Griffin says that as the years go by, one would expect COVID-related deaths to creep down, but not enough is being done to prevent COVID fatalities.
He adds: “We try and bring excess deaths from non-communicable diseases like cancer and obesity, but we don’t seem to do it very well for infectious disease, even though that’s something we can do a lot more about.”
Dr Duncan says that we “urgently need multi-layered public health protections”, including seasonal vaccines and ventilation systems for cleaner indoor air to “stop people continuously re-infected with constantly evolving new variants”.
She adds that “already licenced medications” could help people with long-term COVID complications but the government needs to fund them.
What has COVID taught us?
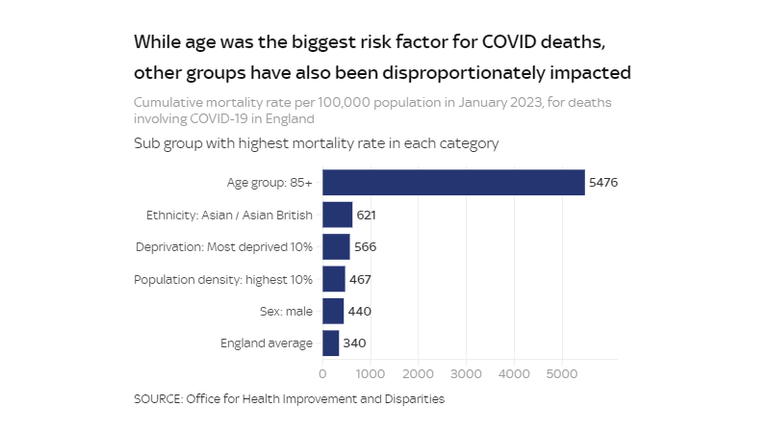
Mr Fell says that as a nation we went into the pandemic in a poor state of health, with “deep inequalities” between ethnic and socioeconomic groups.
“The pandemic reminded us that inequalities in health outcomes are very real and matter enormously,” he says.
“There was more infection in some populations because of underlying health differences, but also things like occupational exposure and overcrowded housing in terms of chains of transmission.”
In those aged 65 and over, Alzheimer’s disease was the most common pre-existing health condition in people who died with COVID. Diabetes was the most common for those under 65.
Although COVID is still a factor driving excess deaths, Mr Fell highlights the mortality rate for age-old public health concerns like smoking, which according to the NHS, causes around 76,000 deaths a year in the UK.
“We still have all the other pandemics of death and illness day in day, out,” he adds. “We need to put as much effort into some of those things as we did in how we responded to COVID.”
From improved ventilation in schools and hospitals to investment in more antiviral drugs and vaccines, Prof Griffin adds: “If you think about the trillions of pounds that have been destroyed by COVID globally, surely the investment of however many million is worthwhile for this and future pandemics.”
Government guidance states that, based on evidence, the vaccine programme changed in 2023 to target higher-risk groups, and that vaccinating children outside of those groups is not recommended.
It also says that data at the end of 2022 suggested almost all older children and adults had coronavirus antibodies from either vaccines or infection.
Sky News has contacted the Department of Health and NHS England for comment.